Atlas RL-eye
Bem vindo !
O Atlas RL-eye é uma base de dados de Oftalmologia, online e de acesso gratuito, editada por especialistas do Centro Cirúrgico de Coimbra.
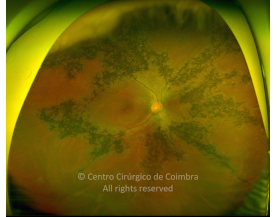
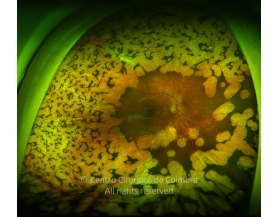
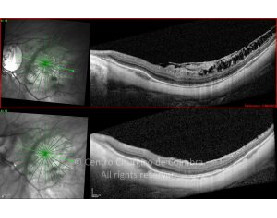
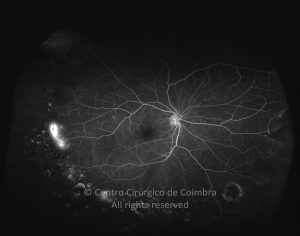
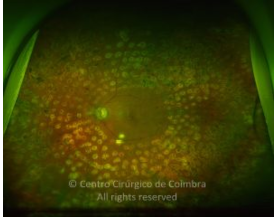
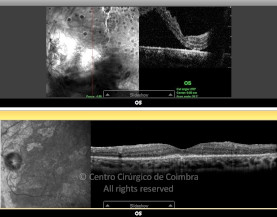
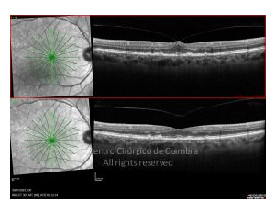
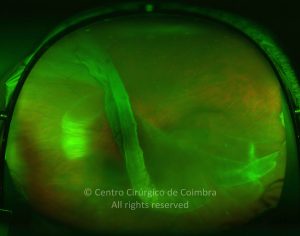
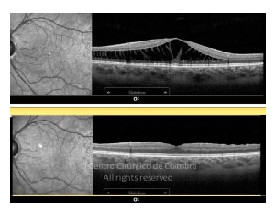
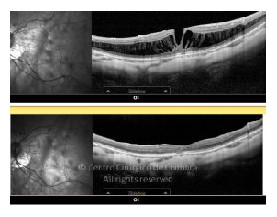
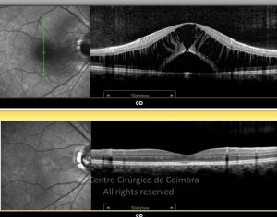
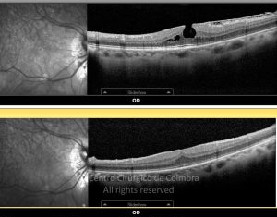
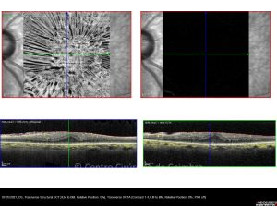
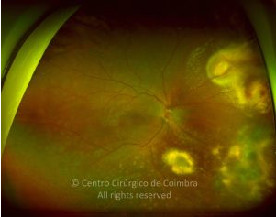
Cada caso clínico é apresentado com todos os Exames Complementares de Diagnóstico, realizados com as mais recentes tecnologias (Zeiss, Heidelberg, Alcon, Sony e Optos). Cada imagem é importante e fundamental na avaliação, conhecimento e acompanhamento de cada doente.
Para além do diagnóstico, mostra-se o tratamento, a cirurgia (quando necessária), a evolução e a recuperação. Torna-se, por isso, um atlas único e poderoso, no ensino e aprendizagem, quer para o doente, ávido de informação fidedigna, quer para estudantes, profissionais de saúde e principalmente para qualquer oftalmologista.
É um atlas em constante progresso e atualização.