Age-related macular degeneration (AMD) is a major public health problem. It is the leading cause of severe central visual acuity loss in developed countries in people over 50 years of age. Initial stages of AMD are characterized by drusen, focal hyperpigmentation or retinal pigment epithelium (RPE) degeneration. Most patients are asymptomatic or complain of mild decrease in visual acuity and metamorphopsias. Two main forms of advanced AMD have been described: dry-AMD, representing 85-90% of patients; neovascular (wet) AMD represents 10-15% of cases. Wet AMD is characterized by the presence of choroidal neovascularization (CNV). CNV develops when a bud of neovascular tissue, arising from the choriocapillaris, grows through a break in Bruch’s membrane and reaches the sub-RPE space. Usually the new vessels are accompanied by fibroblasts and collagen deposits. The end result is the formation of a fibrovascular complex.
Patients may complain of sudden loss of vision, methamorphopsias and a paracentral scotoma.
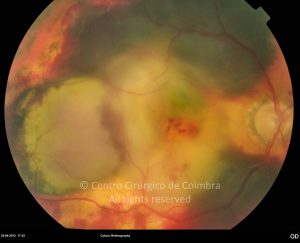
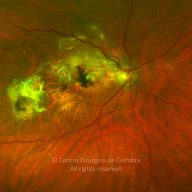
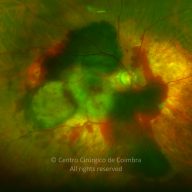
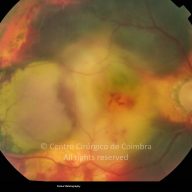
Fundoscopy may reveal subretinal or intra-retinal lipids, fluid or blood. RPE detachment and tears may also occur. Fluorescein angiography is an essential examination for the diagnosis of CNV. Two basic angiographic have been described: the classic and the occult CNV. Indocyanine green angiography (ICG) can offer additional information in cases of occult CNV.
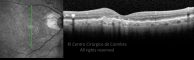
Optical coherence tomography (OCT) is the examination of choice for the follow-up of this group of patients.
Today, the therapy of choice today is intravitreal injection of anti-VEGF agents.
Differential Diagnosis:
- Central serous chorioretinopathy (CSC)
- Pattern Dystrophy
- Drug toxicity.