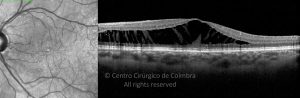
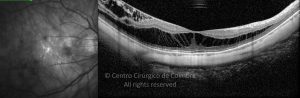
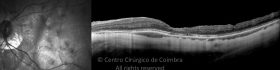
Myopic Foveoschisis (MFS) is a recently recognized clinical entity and one of the causes of visual loss in highly myopic patients. Prevalence has been reported to be 9% to 20% of myopic eyes with staphylomas. MFS can lead to the development of subtle retinal detachments and/or macular holes.
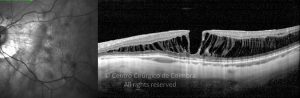
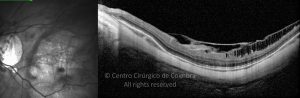
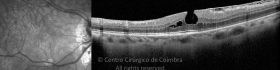
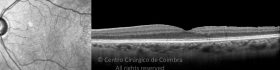
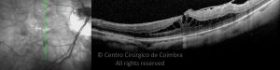
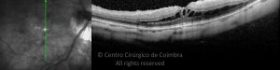
The disease begins with schisis in the inner retinal layers, slowly progressing over the years, to outer retinal layers, and may precede lamellar or full-thickness macular hole formation. Advanced stages of myopic foveoschisis usually involve macular detachment.
The pathogenesis of myopic traction is believed to be multifactorial, involving vitreomacular traction, vitreous cortex remnants, epiretinal membrane, retinal vascular traction, internal limiting membrane rigidity and progression of a posterior staphyloma.
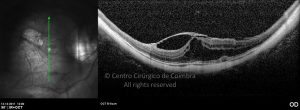
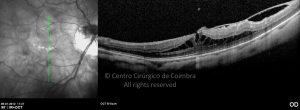
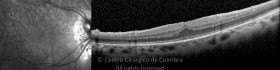
Visual deterioration, epiretinal membrane and macular hole in the context of MFS can be approached, with pars plana vitrectomy with internal limiting membrane peeling and gas tamponade (in cases of associated macular hole) with good results in eyes with myopic traction maculopathy, showing anatomical resolution of foveal schisis .
References:
Galveia, J., Travassos, A., Proença, D., Travassos, A., & Proença, R. (2014). Schisis Miópica – Revisão de 14 Casos Clínicos. Revista Sociedade Portuguesa De Oftalmologia, 37(1).
Gohil, R., Sivaprasad, S., Han, L. et al. Myopic foveoschisis: a clinical review. Eye 29, 593–601 (2015).
Ohno-Matsui, K. (2014). Myopic Macular Retinoschisis. In: Spaide, R., Ohno-Matsui, K., Yannuzzi, L. (eds) Pathologic Myopia. Springer, New York, NY.