Diabetes is a worldwide epidemic disease. In recent decades it has progressed from a disease affecting people primarily in developed countries, to a global phenomenon. Today diabetic retinopathy is a major cause of blindness in adult patients.
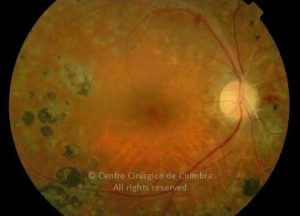
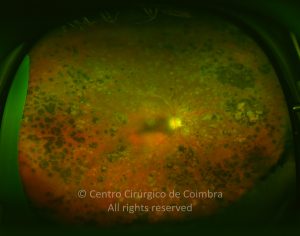
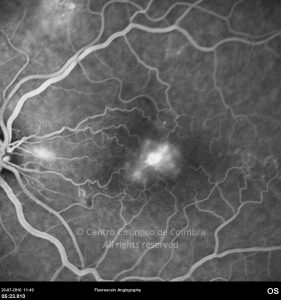
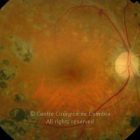
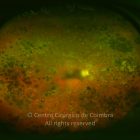
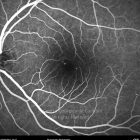
The eye is one of the target organs of this multisystemic disease. Diabetic retinopathy is nothing more than a compromise of the retinal microcirculation. The chronic exposure to hyperglycemia determines a number of biochemical and consequently histological changes. Initially, selective loss of pericytes, basement membrane thickening, as well as a diverse number of hematologic abnormalities, generate capillary occlusion, microaneurysm formation, dilation and beading of retinal veins as well as retinal ischemia.
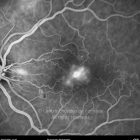
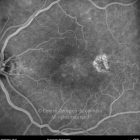
A compromise of the endothelial barrier function allows vascular leakage, originating retinal edema and deposition of hard exsudates. Areas of retinal ischemia generate vasoproliferative factors (mainly vascular endothelium growth factor – VEGF) that later stimulate the growth of neovessels.
According to fundoscopic findings, diabetic retinopathy may be divided in non-proliferative and proliferative diabetic retinopathy, based on the presence of neovascularization. The most commonly used classification scale is the International Clinical Diabetic Retinopathy Disease Severity Scale: