Ocular ischemic syndrome (OIS) is a state of ocular hypoperfusion caused by vascular disease. The most common cause is an ipsilateral atherosclerotic carotid artery disease, producing stenosis. Dissecting carotid aneurisms as well as giant cell arteritis have also been reported as causing critical stenosis of internal or common carotid arteries. When stenosis reaches 70% of the vascular lumen, flow abnormalities can be demonstrated. When stenosis reaches 90% of the carotid lumen, ipsilateral central retinal artery perfusion pressure is reduced by 50%. In rare cases, OIS can be caused by ipsilateral ophthalmic artery obstruction. A case of chronic central retinal artery occlusion may also mimic the findings of OIS.
OIS is more common in males, with a male to female ratio of 2:1. The mean age of diagnosis is 65 years, occurring usually in the 6th to 9th decades of life. It is bilateral in 20% of cases.
Clinically OIS can manifest as a gradual decrease in visual acuity over days to weeks (80%), amaurosis fugax (15%) or sudden loss of vision (12%). Another common complaint is prolonged visual recovery time after exposure to bright light. Ocular or periorbital pain, characterized as dull, is present in 40% of patients (due to either ischemia of the globe, increased intraocular pressure or ischemia of the ipsilateral meninges).
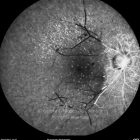
Signs include a decrease in visual acuity and prominent collateral vessels from external to internal carotid artery system. Slit lamp examination may reveal corneal edema, anterior chamber cells or flare, fixed pupil and rubeosis iridis. Intraocular pressure may be elevated (outflow compromise) or low (decreased perfusion of the ciliary body). Posterior segment findings include narrowed retinal arteries, dilated retinal veins, hemorrhages, microaneurysms and neovascularization of the optic disc or elsewhere.