Ocular tuberculosis is an infection caused by Mycobacterium tuberculosis. It can manifest as a primary infection or affect the eye via the hematogenous pathway. About 1-2% occurs through systemic tuberculosis. It may be unilateral or bilateral and occurs in all age ranges.
Tuberculosis can affect any structure in the eye and typically presents as a granulomatous process with multifocal, light colored choroidal granulomas.
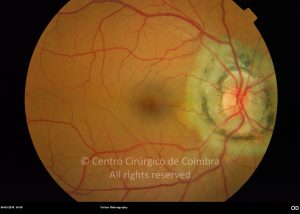
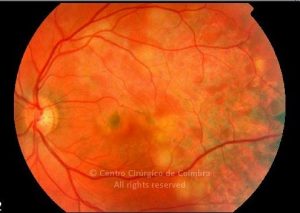
Clinically it manifests as uveitis with a varied clinical presentation, such as chronic iridocyclitis, focal or multifocal choroiditis, and pan-periphlebitis. There can also be exudative retinitis with venous dilatation, hemorrhages and numerous white or yellow superficial exudates. Diffuse choroiditis (the presence of white-yellowish tubers with a diameter of 1/6 to ½ the diameter of the papillae in the choroid) is rare.
Latent tuberculosis causes autoimmune lesions, whether in the form of peripheral retinal vasculitis in young adults or in the form of serpiginous choroiditis. The most common presentation is the appearance of multifocal lesions of choroiditis in the posterior pole and periphery that expand centrifugally and later coalesce in a serpiginoid pattern. The active lesions are yellowish-white, which appear hypo-fluorescent in the early phase of fluorescein angiography and hyper-fluorescent in the late phase.