Diabetes is a worldwide epidemic disease. In recent decades it has progressed from a disease affecting people primarily in developed countries, to a global phenomenon. Today diabetic retinopathy is a major cause of blindness in adult patients.
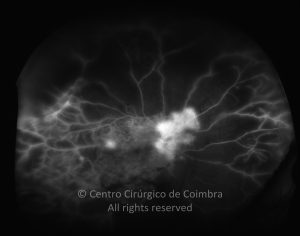
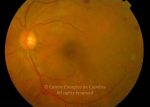
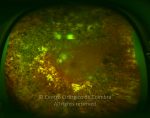
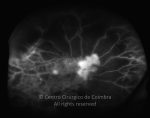
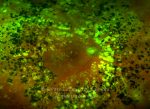
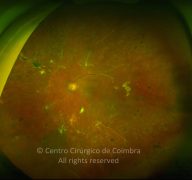
The eye is one of the target organs of this multisystemic disease. Diabetic retinopathy is nothing more than a compromise of the retinal microcirculation. The chronic exposure to hyperglycemia determines a number of biochemical and consequently histological changes. Initially, selective loss of pericytes, basement membrane thickening, as well as a diverse number of hematologic abnormalities, generate capillary occlusion, microaneurysm formation, dilation and beading of retinal veins as well as retinal ischemia.
A compromise of the endothelial barrier function allows vascular leakage, originating retinal edema and deposition of hard exsudates. Areas of retinal ischemia generate vasoproliferative factors (mainly vascular endothelium growth factor – VEGF) that later stimulate the growth of neovessels.
According to fundoscopic findings, diabetic retinopathy may be divided in non-proliferative and proliferative diabetic retinopathy, based on the presence of neovascularization. The most commonly used classification scale is the International Clinical Diabetic Retinopathy Disease Severity Scale:
No apparent retinopathy: no abnormalities
- Mild Non-proliferative Diabetic Retinopathy (NPDR): microaneurysms only
- Moderate NPDR: more than just microaneurysms but less than severe NPDR
- Severe NPDR:
Any of the following:
- More than 20 intraretinal hemorrhages in each of 4 quadrants
- Definite venous beading in 2 or more quadrants
- Prominent intraretinal microvascular abnormalities (IRMA) in at least one quadrant
And no signs of proliferative retinopathy
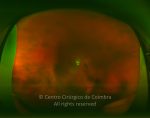
- Proliferative Diabetic retinopathy (PDR):
One or more of the following:
- Neovascularization
- Vitreous/Preretinal hemorrhage
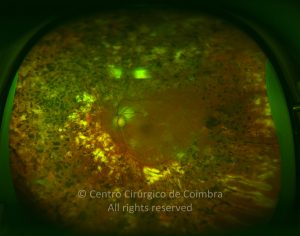
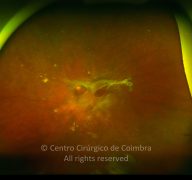
Neovessels in PDR are first intra-retinal with minimal fibrosis After this initial phase they cross the internal limiting membrane (ILM), and migrate to the vitreous body, using it as substrate for further growth. These vessels are accompanied by fibrotic changes, forming pre-retinal membranes, usually along the vascular arcades. The final stage is characterized by an involution of the vascular component and contraction of the fibrotic membranes.
During this cycle, several complications may arise.
- Mild neovessels in the optic disc (NVD) when associated with vitreous hemorrhage
- Moderate to severe NVD (1/4 to 1/3 of the optic disc area), with or without vitreous hemorrhage
- Moderate neovessels elsewhere (NVE) (1/2 the optic disc area), with vitreous hemorrhage.
Treatment should be prompt in this group of patients given the high risk of severe visual loss.
Medical management plays a primordial role in PDR. Optimal glycemic (glycosylated hemoglobin – HbA1c < 7%) and blood pressure control are paramount to a good outcome.
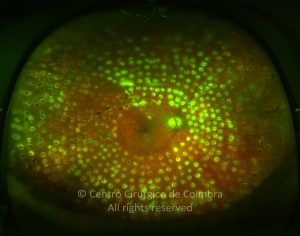
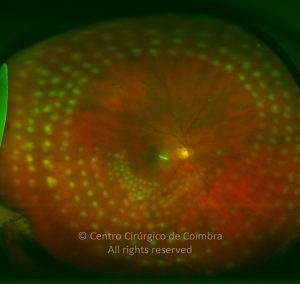
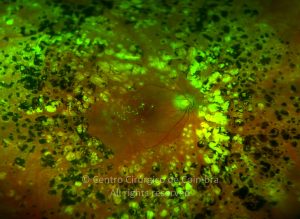
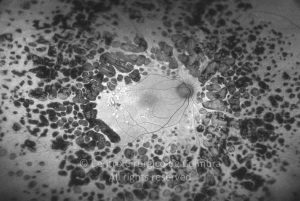
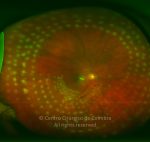
Panretinal photocoagulation (PRP) is the gold standard for patients with severe NPDR and PDR. Laser photocoagulation aims to destroy the ischemic areas of the retina and reduce the production of vasoproliferative factors. Scatter laser should be avoided in areas of vitreo-retinal traction and prominent fibrovascular membranes since it can determine their contraction and subsequent retinal detachment.
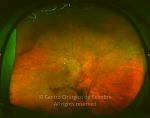
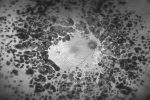
Vitreous hemorrhage is a common occurrence in diabetic patients and frequently heralds the diagnosis of PDR. Blood in the vitreous cavity and its degradation products such as hemosiderin are toxic to retinal structures. A balance should be struck between a conservative attitude, observing the patient regularly and surgical intervention with pars plana vitrectomy (PPV). The Diabetic Retinopathy Vitrectomy Study (DRVS) published in 1985 demonstrated a superiority of early (1-6 months) surgery, when compared to late surgery ( > 1 year) in patients with diabetes type 1. This benefit was not conclusively found for type 2 diabetics. Given the advances in vitreoretinal surgery in the last decades we feel inclined to recommend an earlier intervention that should be made more urgent in patients with type 1 diabetes, patients never submitted to laser photocoagulation, patients with serious diabetic retinopathy in the fellow eye and patients not likely to comply with a regular follow-up regimen.
Intraoperatively, after vitrectomy a thorough PRP with endolaser up to the ora serrata should be performed. One particular entity that demands prompt surgical intervention is pre-macular, retro-hyaloid hemorrhage. A PPV, with induction of posterior vitreous detachment (PVD) and clearance of the pre-retinal blood avoids fibrosis and a subsequent dismal visual prognosis.
Current indications for PPV in diabetic patients include:
- Dense, nonclearing vitreous hemorrhage
- Tractional retinal detachment involving or threatening the macula
- Combined tractional and rhegmatogenous retinal detachment
- Diffuse macular edema associated with taut posterior hyaloids
- Significant recurrent vitreous hemorrhage despite maximal PRP