Retinitis pigmentosa (RP) is a group of hereditary retinal diseases, which are characterized by progressive loss of peripheral vision, and poor night vision (nyctalopia) or poor vision in excessive light, and can later lead to loss of central vision.
There are several types of RP caused by numerous genetic mutations, whose pattern of inheritance can be dominant or recessive. RP is typically a dystrophy of photoreceptor cells in which the genetic defect causes cell death mainly in the rods and, more rarely, in the cones and the retinal pigment epithelium (RPE).
Usually the symptoms start to appear between 10 and 30 and disease progression is variable, presenting tunnel vision in the later stages.
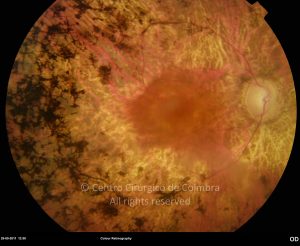
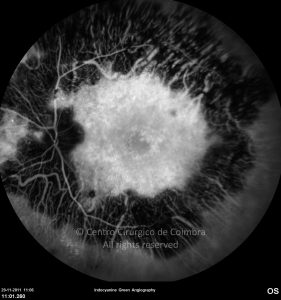
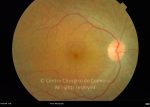
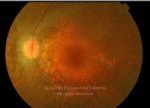
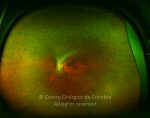
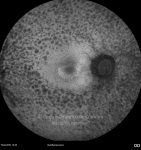
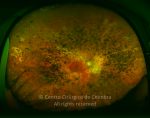
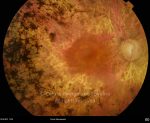
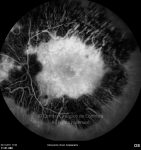
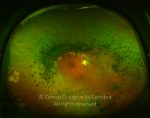
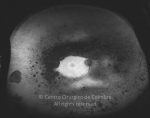
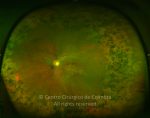
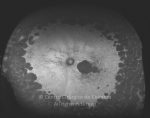
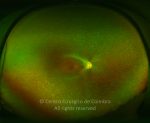
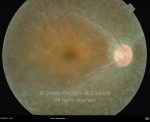
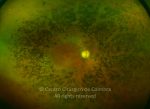
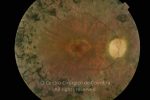
Fundoscopy reveals RPE atrophy and hyper-pigmentation in the periphery of the retina and an average optic disc. The presence of cells in the vitreous is common, and some patients develop cystoid macular edema. The macular pigment changes confer a “bull’s eye” appearance.
Systemic Diseases Associated with Retinitis Pigmentosa:
Systemic diseases associated with retinitis pigmentosa include a wide spectrum of disorders with diverse chromosomal, metabolic, and morphologic findings:
- Alport syndrome
- Bardet-Biedl syndrome
- Kearns-Sayre syndrome
- Mucopolysaccharidosis
- Refsun disease
- Usher syndrome
- Waardenburg syndrome
All of the disorders in this group are genetically determined degenerations or dystrophies and in all of them the progressive degeneration of the photoreceptors leads to a combination of visual field defects, problems with night vision, and problems with central vision.