The uveal melanoma is the intraocular primary malignant neoplasia most common in adults. These tumors are usually unilateral and detected at between 55 and 60 years of age.
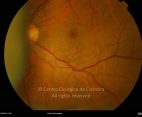
Choroidal melanoma is a solid tumor, ranging from dark brown to golden in color. The earliest pathognomic sign is appearance of orange patches in the pigment epithelium due to accumulation of the lipofuscin In about 20% of cases the tumor breaks through Bruch’s membrane and the retinal pigment epithelium, growing into the retina in the form of a mushroom. It is therefore associated with rhegmatogenous retinal detachment and subretinal edema. Initially patients are asymptomatic but may have blurred vision, visual field defects, flashes and floaters. Most patients with melanoma of the choroid are submitted to radiotherapy as enucleation is reserved just for advanced cases.
Ciliary body melanoma is another subtype of uveal melanoma, generally with a worse prognosis. Iris melanomas form only a small proportion of all uveal melanomas and may be circumscribed or diffuse. Circumscribed melanomas have a nodular shape and have a good prognosis.